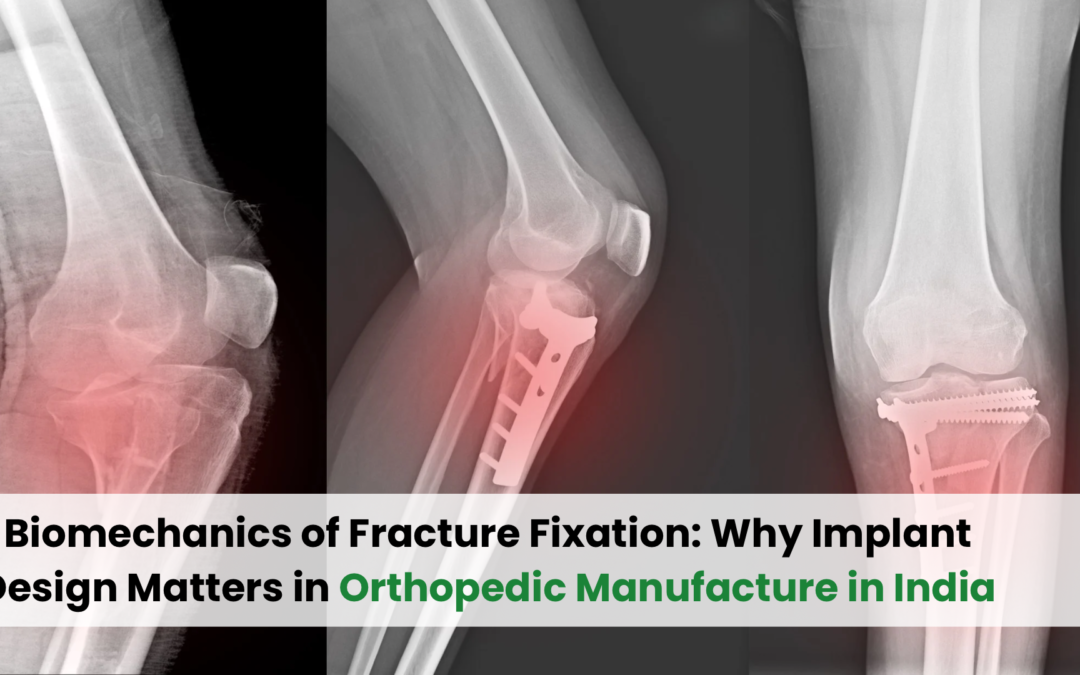
In the realm of orthopedic trauma care, fracture fixation is not merely about placing screws and plates—it’s a precise science deeply rooted in biomechanics. The way implants are designed, shaped, and manufactured plays a pivotal role in how effectively a bone heals and regains its natural function. In recent years, the rise of orthopedic manufacture in India has significantly contributed to advancing this field by creating implants that are both biomechanically sound and globally competitive.
This article delves into the biomechanics of fracture fixation and why implant design—especially in the context of India’s growing orthopedic industry—matters more than ever.
Understanding the Biomechanics of Fracture Fixation
Biomechanics refers to the study of how forces affect biological systems—in this case, the musculoskeletal system. When a bone breaks, it loses its structural integrity. The goal of fracture fixation is to restore this integrity by using mechanical devices (implants) that absorb and redistribute physiological forces during the recovery process.
Key Biomechanical Goals of Fracture Fixation:
- Stability: Ensuring the fractured bone fragments remain aligned under body weight and movement.
- Load Sharing vs. Load Bearing: Determining whether the implant shares the mechanical load with the bone or completely bears it during recovery.
- Micro-motion Management: Allowing limited movement that promotes callus formation without compromising alignment.
- Stress Distribution: Preventing stress concentration that can lead to implant failure or re-fracture.
Each of these goals is directly influenced by implant design—from the material used to the shape, size, thread type, and locking mechanism.
Why Implant Design Matters
Not all fractures are the same—and neither are the bones they occur in. A flat tibial plateau fracture requires a different fixation strategy than a spiral humeral shaft break. Hence, implant design must be tailored to both the location and nature of the fracture.
Factors That Influence Implant Performance:
- Material Strength and Elasticity: Titanium alloys and stainless steel are preferred due to their combination of durability and flexibility.
- Geometry and Profile: Low-profile plates reduce soft tissue irritation, while anatomical contours improve bone-implant interface.
- Locking Mechanism: Locking plates provide angular stability, essential for osteoporotic or comminuted fractures.
- Screw Configuration: Direction, spacing, and size of screw holes affect how forces are transmitted across the fracture site.
A well-designed implant not only stabilizes the bone but also encourages biological recovery, reduces the need for secondary surgery, and enhances patient mobility.
The Role of Orthopedic Manufacture in India
India has emerged as a key player in orthopedic implant manufacturing, combining cost-efficiency with innovation. The country’s manufacturers are not just producing basic trauma implants—they are investing in biomechanical research, precision engineering, and global regulatory standards.
India’s Strengths in Orthopedic Manufacturing:
- Affordable Innovation: Indian implants offer world-class quality at a fraction of Western prices.
- CE and USFDA Approvals: Many manufacturers now comply with international certifications, making Indian implants export-ready.
- Design Customization: Advances in 3D modeling and CAD tools allow for custom-fit implants based on patient anatomy.
- R&D Focus: Partnerships with medical colleges and orthopedic surgeons help refine implant designs based on real-world use.
The growing emphasis on biomechanically optimized implants is placing India at the forefront of fracture fixation solutions for both domestic and global markets.
Popular Implant Types Designed with Biomechanics in Mind
- Locking Compression Plates (LCP): Combine stability and compression, useful in osteoporotic bone.
- Intramedullary Nails: Used in long bones, allow for load-sharing and early mobilization.
- Dynamic Hip Screws: Enable controlled collapse at the fracture site, essential for recovery in hip fractures.
- Cannulated Screws: Allow for minimally invasive insertion, ideal for small bone fractures.
These implants are being designed and manufactured across India with increasing attention to biomechanics and clinical outcomes.
How Surgeons Benefit from Biomechanically-Sound Implants
Orthopedic surgeons choose implants not just for their shape or brand, but for how they perform inside the body. A good implant design can:
Reduce surgery time
Lower post-operative complications
Promote faster recovery
Minimize hardware failure
Improve patient satisfaction
When orthopedic manufacture in India focuses on biomechanical principles, it empowers surgeons with tools that elevate the standard of trauma care.
Challenges and Opportunities
Despite its growth, India’s orthopedic sector still faces challenges such as:
- Ensuring uniform quality across manufacturers
- Investing more in biomechanics education
- Expanding into 3D-printed, patient-specific implants
- Competing with global giants in branding and perception
However, the opportunity to lead in cost-effective, biomechanically superior implants remains enormous. With increasing collaboration between engineers, clinicians, and regulatory bodies, India is well-positioned to shape the future of fracture fixation.
Conclusion
Fracture fixation is as much a biomechanical endeavor as it is a surgical one. The success of treatment depends not only on the skill of the surgeon but also on the design and reliability of the implant. As the field evolves, implant design must continue to prioritize mechanical performance, anatomical accuracy, and biological compatibility.
The rise of orthopedic manufacture in India is playing a pivotal role in this evolution—delivering implants that are affordable, precise, and aligned with global standards. By embracing biomechanics at the core of implant design, India is not only recover bones but also setting new standards in orthopedic excellence.